Emerging and Communicable Diseases
This page provides information and resources on emerging or communicable diseases highlighted by the Health Department.
Monkeypox Virus (mpox)
In the spring of 2023, the CDC began investigating a cluster of mpox cases in the Chicago area. From April 17 to May 5, 2023, a total of 12 confirmed and one probable case of mpox were reported to the Chicago Department of Public Health. All cases were among men, all had symptoms, and nine - or 69% of the cases - had received 2 JYNNEOS vaccine doses.
The CDC anticipates that the spring and summer seasons of 2023 could lead to a resurgence of mpox as people gather for festivals and other events. See below for vaccine recommendations, signs, symptoms and how to prevent the spread of mpox.
Mpox vaccine information
There is a vaccine available to prevent the spread of mpox(PDF, 174KB) . Currently, CDC does not recommend routine immunization against mpox for the general public.
Mpox vaccination should be offered to people with high potential for exposure to mpox:
- People who had known or suspected exposure to someone with mpox.
- People who had a sex partner in the past 2 weeks who was diagnosed with mpox.
- Gay, bisexual, and other MSM, and transgender or nonbinary people (including adolescents who fall into any of these categories) who, in the past 6 months, have had
- A new diagnosis of one or more sexually transmitted diseases (e.g., chlamydia, gonorrhea, syphilis).
- More than one sex partner
- People who have had any of the following in the past 6 months
- Sex at a commercial sex venue
- Sex in association with a large public event in a geographic area where mpox transmission is occurring.
- Sex in exchange for money or other items
- People who are sex partners of people with the above risks
- People who anticipate experiencing any of the above scenarios
- People with HIV infection or other causes of immunosuppression who have had recent or anticipate potential mpox exposure
- People who work in settings where they may be exposed to mpox
- People who work with orthopoxviruses in a laboratory
If you are interested in getting a vaccination, contact the Health Department at 708.358.5480 or email health@oak-park.us.
Signs and symptoms
Most people with mpox will get a rash.
- The rash may be located in areas like the hands, feet, chest, face, on or near the genitals or anus
- The rash will go through several stages, including scabs, before healing.
- The rash can look like pimples or blisters and may be painful or itchy.
- The rash may also be inside the body, including the mouth, vagina, or anus
Images of an Mpox Rash
Content note: some of the pictures could be considered graphic by some.
Some people have developed a rash before (or without) flu-like symptoms.
- The flu-like symptoms may include fever, headache, muscle aches and backache, sore throat, cough, swollen lymph nodes, chills, or exhaustion.
- If someone has flu-like symptoms, they will usually develop a rash 1-4 days later.
Mpox symptoms usually start within 3 weeks of exposure to the virus.
The illness typically lasts 2-4 weeks. Sometimes, people get a rash first, followed by other symptoms. Others only experience a rash.
How mpox spreads
At this time, mpox is spreading mostly through close, intimate contact with someone who has the virus.
The virus can spread from person-to-person through direct contact with the infectious rash, scabs, or body fluids. It also can be spread by respiratory secretions during prolonged, face-to-face contact, or during intimate physical contact, such as kissing, cuddling, or sex. In addition, pregnant people can spread the virus to their fetus through the placenta.
Touching items (such as clothing or linens) that previously touched the infectious rash or body fluids is another way mpox spreads.
People who do not have mpox symptoms cannot spread the virus to others.
Mpox can spread from the time symptoms start until the rash has fully healed and a fresh layer of skin has formed.
Preventing the spread
- Avoid close, skin- to- skin contact with people who have a rash that looks like mpox.
- Do not touch the rash or scabs of a person with mpox.
- Do not kiss, hug, cuddle or have sex with someone with mpox.
- Do not share eating utensils or cups with a person with mpox.
- Do not handle or touch the bedding, towels, or clothing of a person with mpox.
- Wash your hands often with soap and water or use an alcohol-based hand sanitizer.
What to do if you get sick
- Isolate at home
- If you have an active rash or other symptoms, stay in a separate room or area away from people or pets you live with, when possible.
- The CDC recommends vaccination for people who have been exposed to MPV and people who are at higher risk of being exposed to mpox.
2022 Local mpox status reports
Beginning in May 2022, health organizations across the globe, including the Centers for Disease Control and Prevention, began tracking cases of Monkeypox virus (mpox), which began to spread across several countries that don't normally report cases. In August of 2022, the U.S. Department of Health and Human Services (HHS) declared a Public Health Emergency regarding mpox in order to strengthen and accelerate the response from the public health sector. The Oak Park Health Department began to accept calls related to MPV that month, between August 2022 and January 2023, the department investigated 8 potential cases. These investigations led to 22 people being vaccinated against mpox. In December of 2022, HHS said that it would not renew the declaration of the public health emergency when it expires January 31, 2023.
See below for the status reports produced by the Health Department during this public health emergency on the Village of Oak Park's operational activities in response to MPV that were issued to the Village Board as necessary. Click on the titles below to view the report:
- February 3, 2023(PDF, 138KB)
- December 30, 2022(PDF, 136KB)
- December 2, 2022(PDF, 134KB)
- November 18, 2022(PDF, 134KB)
- November 11, 2022(PDF, 133KB)
- November 4, 2022(PDF, 133KB)
- October 28, 2022(PDF, 109KB)
- October 21, 2022(PDF, 109KB)
- October 14, 2022(PDF, 108KB)
- October 7, 2022(PDF, 108KB)
- September 30, 2022(PDF, 115KB)
- September 23, 2022(PDF, 85KB)
- September 16, 2022(PDF, 84KB)
- September 9, 2022(PDF, 90KB)
- September 2, 2022(PDF, 83KB)
- August 26, 2022(PDF, 82KB)
- August 19, 2022(PDF, 81KB)
Influenza (Flu)
Flu is a contagious respiratory illness caused by influenza viruses that infect the nose, throat, and sometimes the lungs. It can cause mild to severe illness, and at times can lead to death. The best way to prevent flu is by getting a flu vaccine each year.
How Flu Spreads
Most experts believe that flu viruses spread mainly by tiny droplets made when people with flu cough, sneeze, or talk. These droplets can land in the mouths or noses of people who are nearby. Less often, a person might get flu by touching a surface or object that has flu virus on it and then touching their own mouth, nose or possibly their eyes.
People at Higher Risk for Severe Outcomes as a Result of Flu
Anyone can get flu (even healthy people), and serious problems related to flu can happen at any age, but some people are at higher risk of developing serious flu-related complications if they get sick. This includes people 65 years and older, people of any age with certain chronic medical conditions (such as asthma, diabetes, or heart disease), pregnant people, and children younger than 5 years.
Preventing Seasonal Flu
The first and most important step in preventing flu is to get a flu vaccine each year. Flu vaccine has been shown to reduce flu related illnesses and the risk of serious flu complications that can result in hospitalization or even death. CDC also recommends everyday preventive actions (like staying away from people who are sick, covering coughs and sneezes, and frequent handwashing) to help slow the spread of germs that cause respiratory (nose, throat, and lungs) illnesses, like flu.
Below are a few graphs showing a cluster of flu cases and hospitalizations around the months of November and December, which is typical "flu season" because people tend to find themselves indoor more frequently. There are notably more cases this fall compared to last fall.
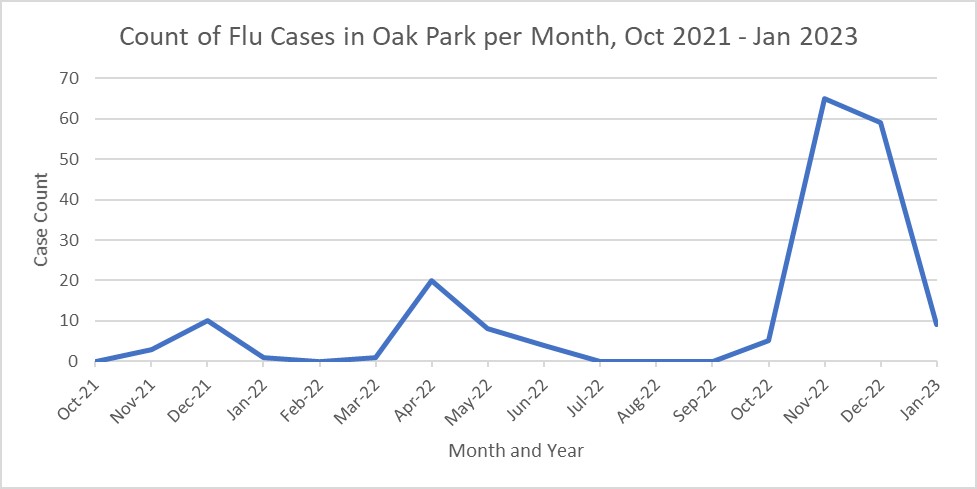
In the U.S., most flu activity starts in October and ends in May. Peak flu season is typically between December and March. Comparing our current flu season to last year's, there is a greater number of cases this season so far. The Oak Park Health Department continues to encourage flu vaccination and other behaviors to minimize the spread of the flu, including staying home when sick and frequent handwashing.
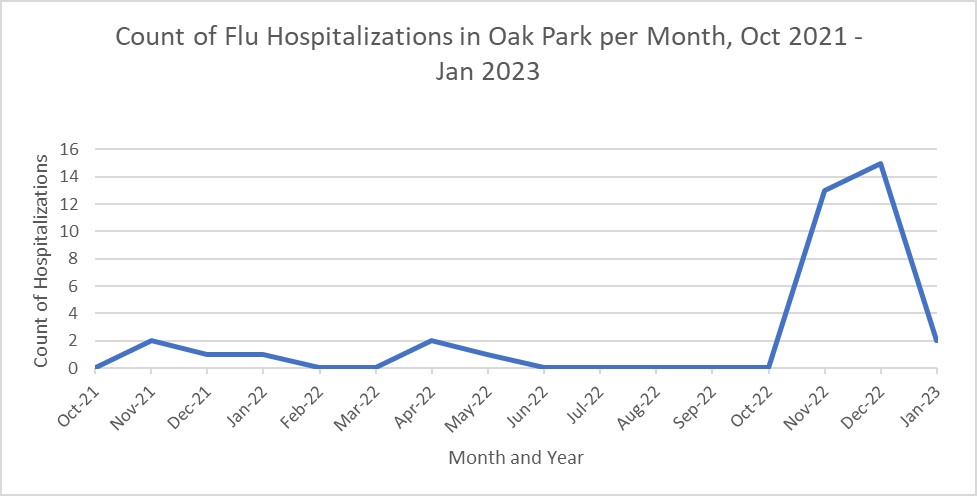
As illustrated in the graph above, this year's flu cases have been more severe and resulted in an increase in hospitalizations. Taking the precautions listed above can help protect populations more vulnerable to severe cases that require hospitalization.
Ebola
In September 2022, an outbreak of Ebola was identified in Uganda. At this time, there are no cases of Ebola in the United States and Ebola does not pose a great health risk to the people of Oak Park. Since late September, the U.S. Centers for Disease Control and Prevention (CDC) and Customs and Border Protection (CBP) have been screening travelers at major airports, including O'Hare, who have been in countries most affected by the Ebola outbreak, which is primarily Uganda.
The Oak Park Health Department is monitoring the situation and will notify the public should there be any cause for action. Below is more information about the Ebola virus.
What is Ebola, signs and symptoms
What is Ebola?
Ebola is a severe disease that is caused by the Ebola virus.
What are the signs and symptoms of Ebola?
Symptoms may appear anywhere from two to 21 days after contact with the virus. Most people will begin to experience symptoms within eight to 10 days. The course of the illness typically progresses from "dry" symptoms initially (such as fever, aches and pains, and fatigue), and then progresses to "wet" symptoms (such as diarrhea and vomiting) as the person becomes sicker.
How does Ebola spread?
Ebola is spread through direct contact with blood or body fluids of a person who is sick with Ebola, or a person who has recently died from Ebola.
What are "body fluids"?
Examples include:
- urine
- saliva
- sweat
- feces
- vomit
- semen
What is "direct contact"?
This means that body fluids, such as those listed above, from an infected person (alive or dead) have touched someone's eyes, nose, mouth or an open cut, wound or abrasion.
Ebola can also be spread on objects or surfaces contaminated with blood or body fluids of an infected person.
A person who is NOT experiencing symptoms, such as fever, vomiting or diarrhea, cannot transmit the virus. Ebola is NOT spread through the air, water or food.
How long does Ebola live outside the body?
Ebola is killed with hospital-grade disinfectants such as household bleach. Ebola on dried surfaces, such as doorknobs and countertops, can survive for several hours; however, virus in body fluids (such as blood) can survive up to several days at room temperature.